Curriculum
The purpose of the respiratory medicine curriculum is to guide the training of speciality trainees who are aiming for dual certification in respiratory and internal medicine.
Completion of training will provide them with the knowledge and skills to manage a full range of general medical and acute and chronic respiratory problems at the level expected of an independent unsupervised practitioner. This will ensure they have the capabilities required to acquire a certificate of completion of training in Respiratory and Internal Medicine and allow them to apply for an NHS consultant post.
Further information about the Respiratory Medicine curriculum can be found on the JRCPTB website links below.
South West Hospitals
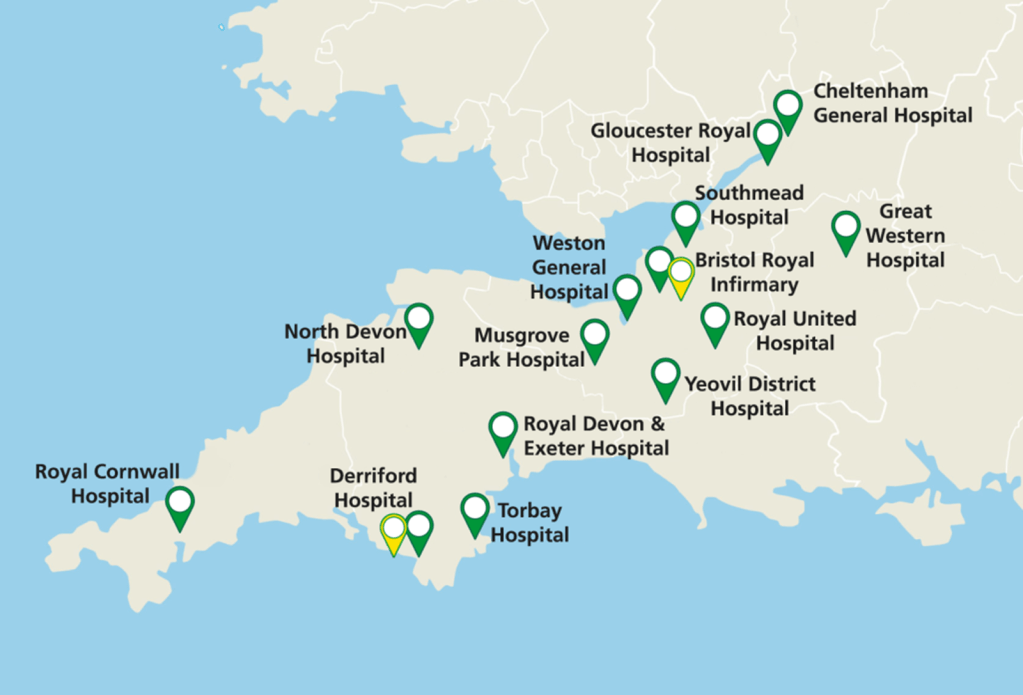
The South West respiratory rotation includes 37 posts in the following hospitals (approximate numbers of registrar posts in brackets):
University Teaching Hospitals:
Bristol Royal Infirmary (4)
Southmead Hospital, Bristol (4)
Royal Devon and Exeter Hospital, Exeter (3)
Derriford Hospital, Plymouth (4 plus 1 ITU)
Royal Cornwall Hospital, Truro (3)
District General Hospitals:
Gloucester Royal Hospital (2)
Cheltenham General Hospital (2)
Great Western Hospital, Swindon (4)
Royal United Hospital, Bath (4)
Musgrove Park Hospital, Taunton (3 plus 1 ITU)
Yeovil District Hospital (1)
Torbay Hospital (2)
North Devon District Hospital, Barnstaple (1)
Respiratory Medicine dual accredits with General Internal Medicine GIM.
This programme aims to provide a very high quality of Respiratory Medicine training. Trainees will be appointed to the rotation, not to specific hospitals. The first post is as described in the advert, thereafter posting will be arranged by the TPD taking into account firstly the training requirements of all the trainees, then specific individual requirements and finally personal preferences. However, wherever possible trainees will only be asked to make one major move within the rotation. A period of OOPE for research or sub-specialty training is encouraged. ICU and thoracic surgery experience are both available in several centres.
For more information, visit:
http://www.medicine.severndeanery.nhs.uk/about-us/respiratory-medicine/
Indicative Trainee Job Plan
Whilst the formal Structured Training Programme is designed to provide much of the knowledge required for expert practice in Respiratory Medicine, a large proportion of training is ‘on-the-job.’ An indicative job plan for a trainee in Respiratory Medicine, as suggested by the Respiratory Curriculum, is as follows:
- Two consultant-led ward rounds per week
- One trainee-led ward round per week
- Two outpatient clinics per week
- One practical procedures session (usually, but not exclusively, bronchoscopy) per week
- Appropriate protected time for essential educational activities should be agreed between the trainer and trainee
It is emphasised that this is intended only as a guide to the general job plan for the average post. It is not expected that this should be rigidly adhered to in all circumstances.
ARCP

The Annual Review of Competence Progression (ARCP) is the formal method by which a trainee’s progression through her/his training programme is monitored and recorded each year. ARCP is not an assessment – it is the review of evidence of training and assessment.
The curriculum states that, in addition to the components of the ePortfolio (meetings, workplace-based assessments, MSF, teaching observations, MCR and audit assessment), trainees should gather evidence of:
- An anonymised record of bronchoscopy experience, including details of exact techniques used, for example, transbronchial biopsy and transbronchial needle biopsy, as well as a record of the positive histology rate for visible tumour.
- An anonymised record of pleural interventional experience.
- An anonmyised record of NIV experience.
- Formal sign off of their NIV competence (perhaps best done as DOPS, mini-CEX and relevant courses)
- Formal sign off of their Intensive Care Medicine experience (could be end of placement appraisal, letter from supervisor etc)
- Details of training in appropriate specific subject areas within Respiratory Medicine, such as lung cancer and sleep breathing disorders (captured in clinic log and mini-CEX and CBD in specialist posts)
- Details of special interest training, particularly in transplantation, pulmonary hypertension, adult cystic fibrosis, domiciliary NIV and occupational and environmental disease.
Please ensure that anything uploaded to the personal library section of your ePortfolio is clearly labelled. Anything that eases the job of the ARCP panel will be much appreciated!
Leadership and Management
Trainees who are in the later stages of training should reflect on how they can demonstrate competency in the above areas and seek opportunities to join committees, identify areas of service improvement, contribute to business plans etc. Demonstration of such knowledge and skills will be essential for attaining a Consultant position.
Trainees may find the following resources helpful in understanding the changing NHS landscape:
- An alternative guide to the new NHS in England from The King’s Fund on Vimeo.
- The NHS Structure explained (NHS Choices)
- The Nuffield Trust guide to the new NHS structure
Completion of a recognised management training course is a mandatory requirement for training. Some options for completing this training can be found on the Courses and Opportunities page.
Teaching and Training
The GMC expects all doctors to demonstrate skills in teaching and training.
The Respiratory Curriculum suggests ways in which trainees might become involved in teaching, which may benefit their own learning (these would therefore be good things to capture in the ePortfolio):
- Teaching medical students, junior doctors & allied health care professionals affords an excellent opportunity to learn
- Presenting at grand rounds or similar clinical meetings provides the opportunity for in-depth study of a particular subject area
- Participation in journal clubs fosters critical thinking and an approach to the evaluation of the medical literature, which is essential for professional practice
- ST3+ trainees will be expected to carry out some assessments on their more junior colleagues from time to time, for example carrying out work place based assessments, and should be specifically trained to do so. Make sure you select ‘keep a record’ when you complete assessments for trainees so you can prove your involvement in training
- All NHS Consultants should be excellent teachers. All trainees should strongly consider attending a formal training for teaching course. Some trainees may wish to become more expert teachers/trainers and to “specialise” in this area when they become a Consultant. They may therefore wish to consider undertaking a more formal training programme and qualification in medical education
Trainees are strongly recommended to attend a formal ‘Training for Teaching’ course. Those with a specialist interest in Medical Education may consider a PGCert, Diploma or Masters in Medical Education. For more information see the Courses and Opportunities page.
PYA
Your PYA should happen in your penultimate year of training, with plenty of time to identify any knowledge or skills gaps. Start thinking about it and getting it organised 18 months before your CCT date. Remember that you need to have 2 PYAs – one for GIM and one for Respiratory Medicine. Make sure HEE arrange both, which are likely to be on different days.
For PYA it is wise to leave one or two outstanding requirements that you can then arrange to do in your last year. Ideally have these booked when you go to PYA so that you can give them a list of outstanding requirements. They are then much less likely to pick something random and difficult for you to do. Of course this means you need to make sure you have done most of the things on the ARCP decision aid before PYA, so stay on top of it throughout training.
Top Tips
- Know the decision aids really well (see link above). Ensure you are up-to-date with all your workplace based assessments.
- Check carefully that you have fulfilled the requirements for procedure sign-off. Ensure you select ‘summative, life-threatening’ where relevant.
- Check your educational supervisor has confirmed your competence of spirometry, lung function interpretation and chest x-ray interpretation (signed off on the curriculum pages)
Other things not specifically highlighted on decision aid but still essential:
- Evidence of training in safe sedation – this requires a course (e.g. bronchoscopy training course in ST4) and formal sign off of your competency with a DOPS
- Subspecialty experience in Pulmonary Hypertension, CF, Occupational Lung Disease and Transplant as per the JRPCTB guidelines
- Integrated care – go on a home visit with the COPD community team and attend PR and write reflections
- HIV –arrange a clinic visit in a HIV service and write a reflection. Make sure you include patients with HIV and Respiratory complications in your CBDs etc
- Genetic and developmental lung diseases – should be covered in a regional training day, and in your CF visit/placement. Try to attend a transition clinic and/or joint immunology clinic and write a reflection/get a CBD.
Before each PYA
Remember that you will need to have separate Respiratory and GIM PYAs. Your assessor may look at your ePortfolio in advance, so make sure it is ready for review a month before PYA.
Prepare your ePortfolio
- Set up new folders within your personal library on the ePortfolio called ‘Respiratory PYA paperwork’ and ‘GIM PYA paperwork’.
- Ensure that the summary of clinical experience (SOCE) form is completed and uploaded to the above folder(s). SOCE form available on JRPTB website.
- Ensure that an up to date CV is uploaded to the above folder(s).
- Ensure that your ePortfolio is up to date so that the assessor can check your progress.
- Make sure any paperwork related to OOP is uploaded, including pre-approval of counting OOP towards training
- Upload a Form R as you would usually do for an ARCP
- Prepare a PYA presentation
On the day of PYA
You will receive an invitation to your PYA which will remind you of the forms you need to upload, as listed above.
For GIM:
It will also ask you to prepare a PYA PowerPoint presentation. This is not stated anywhere on the JRPCTB website. The guidance from HEE is that the presentation should be:
- 5-10 minutes in length
- no more than 6 slides
- detailing your experience on the relevant programme
- relating specifically to the sub-sections of the curriculum, your goals and any outstanding issues for the remaining period until your CCT date
Good luck!
OOPs
A trainee e may take a period of time out of their programme to undertake a period of research or training, gain clinical experience or as a career break. Trainees are required to obtain formal approval from their deanery/LETB to take time out of programme and will not normally be agreed until a trainee has been in programme for at least 1 year. Trainees are not allowed to pursue OOP activities in their final year.
Deaneries/LETB generally ask for requests for OOP to be submitted at least 6 months prior to your start date and after discussion with your ES and TPD.
Types of OOP category (detailed descriptions are available in The Gold Guide):
- OOPR – Time out of programme for research: A period of research may be undertaken often for a higher degree (e.g.: MD, PhD). Up to 12 months credit may be included towards your CCT.
- OOPT – Time out of programme for training: A trainee may gain opportunity to undertake training outside of their regular training programme either in the UK or abroad. The SAC will review how much credit may be provided towards your CCT. This also includes a period of acting up as a consultant.
- OOPE – Time out of programme for clinical experience: A trainee may gain experience similar to OOPR or OOPT, but not approved by the GMC or outside the curriculum e.g. work overseas for voluntary organisations. There is therefore not the ability to credit this period towards your CCT.
- OOPC – Time out of programme for career breaks: It may occur for a variety of reasons including a period of parental, sick or exceptional leave. This is normally limited to 2 years.
Be aware that no credit can be awarded for time OOP without JRCPTB approval and approval cannot be granted retrospectively – it must be applied for and granted by the JRCPTB/GMC prior to OOP.